Dis-Functional Relationship and the SRS
The following case study illustrates the relationship of a remote spondylogenic reflex syndrome (SRS) to pre-existing lumbar pathology, compromised spinal biomechanics, aberrant functional neurology and loss of performance in an elite athlete.
Case Study
A 36-year-old female marathon and trail runner presents two weeks prior to an Imogene Pass Run (Colorado) unable to perform. She developed progressive and debilitating right lower extremity pain and dysfunction over the previous year while training for this and other running events. Her complaint progressed into unrelenting right buttock pain, burning in the right posterior thigh and right hamstring muscle spasms.
A medical evaluation diagnosed her with a tight hamstring muscle and she was prescribed three months of physical therapy in which PT lumbar spinal manipulation further aggravated her complaint.
Her MR revealed an L5/S1 Grade II spondylogenic spondylolisthesis (SS) w/ moderate lumbar degenerative changes in excess of her age. A steroid injection was administered providing moderate relief while continued spinal manipulation (PTM) aggravated her condition further. A second injection proved ineffective.
Her initial SRA chiropractic evaluation revealed a spondylogenic reflex syndrome (primary unstable zygapophyseal joint) at the C4 right intersegmental level.
Specific chiropractic adjusting administered to C3 and C4 motor unit only, resulted in significant reduction in SRS driven psoas muscle facilitation at the L5 level. In essence, SRS based C4R CMT resulted in a notable reduction in L5 neurocompression and thereby mitigated the majority of hamstring over facilitation and its associated metabolic fatigue, pain and causalgia.
Following treatment, the patient was not only able to complete the 17.1 mile run over the 13,114 ft. mountain pass with marginal discomfort; she ranked first in her age group and achieved her best time to date.
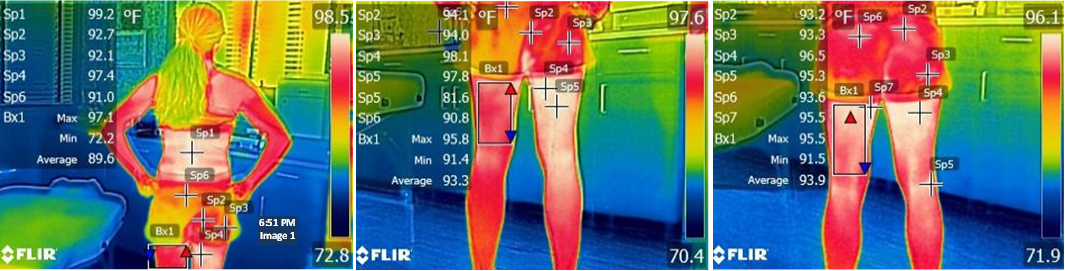
Images 1-3 Infrared temperatures in images 1 and 2 reflect joint and muscle inflammation due to spondylogenic reflexive facet compression and muscle over-facilitation. Suspect muscles include biceps femoris and gracilis.
Image 1 - Pre Treatment IR Image 1, Sp1 references a focal infrared inflammatory profile at the L4/L5 level with a max temperature of 99.2 ‘F. This is well above the average 86-94 degree resting temperature of normal paraspinal muscle and skin surface.
Image 2 - Pre Treatment IR Image 2, Sp4 for the right thigh is 98.1 ‘F compared to left thigh noted in Bx1, having a Max temperature of 95.8 ‘F. This indicates that right hamstring metabolism is operating at 2.3 ‘F higher than the left.
Image 3 - Post Treatment IR Image 3, SP4 illustrates a change in location and max temperature in the right hamstring to 96.5, ‘F i.e. a reduction and shift in static postural metabolic activity of 1.6 ‘F at 30 minutes after treatment when comparing Image 2 to Image 3. Note that left Bx1 metabolism remains relatively unchanged in Image 3 after treatment (.3 degrees difference).
Discussion
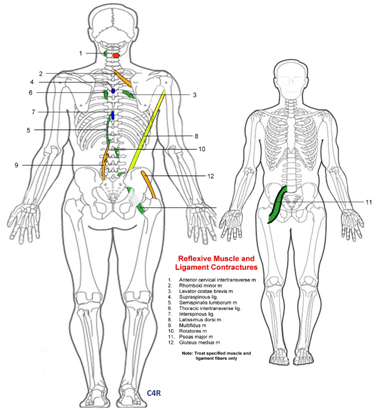
In this example, a C4 spondylogenic reflex dictates that over-facilitation occurs in the psoas and gluteus med. muscles on the ipsilateral L5 side (see image 4).
Chronic psoas induced L5 zygapophyseal loading further aggravates the patient’s underlying pathology by increasing strain and structural instability at the L5/S1 spondylogenic spondylolisthesis level.
Persistent, reflexive L5/S1 facet overloading induces edematous, periarticular hydrostatic nerve root compression at the same level; which in turn results in motor or hamstring facilitation as measured by muscle shortening, muscle metabolic fatigue, weakness, pain and a net performance loss.
Reestablishing normal SRS biomechanics through specific CMT procedures, and/or high frequency/high power deep laser therapy and facet stabilization exercises can remediate a wide array of SRS driven symptoms and conditions.
In this case: predisposing factors to include spondylogenic spondylolisthesis, degenerative joint changes and repetitive motion loading associated with her sport are known causative and complicating factors. Based on this and other similar cases, I believe that our profession is underestimating the complexity of the SRS and its dynamic role as causative, aggravating and/or remedial to the patient’s functional status through intrinsic cord-mediated neurology.
Summary
SRA diagnostic and treatment strategies predictably and consistently defy conventional expectations in post provocative testing, MR findings, physiological responses, and both subjective and objective patient response curves.
At a minimum, identifying and treating the SRS attests to the power of the body’s adaptive response system to maximize functional status even under the worst of physical limitations. Maximizing this strategic asset requires continued research and further understanding of the pathological process and its critical role in clinical outcomes and the patient’s health and wellness.
Image 4 - SRS Correlate to HX and Physical Findings Image 4 illustrates the primary driving spondylogenic reflex (C4R) and reflexively facilitated core muscles. Note the C4R SRS (red), its psoas muscle facilitation relationship (muscle #11) and its potential for neuroforaminal compression.